CORRESPONDENCIA
María del Mar Calvo Bernal
Torrecárdenas University Hospital Complex. Almeria.
04009 Almeria
CITA ESTE TRABAJO
Calvo Bernal MM, Rodriguez Mateu A, Moreno Moraleda I, Gil Belmonte MJ. Chronic diarrhea secondary to intestinal spirochetosis, should we think about it? RAPD 2024;47(2):80-83. DOI: 10.37352/2024472.4
Introduction
Human intestinal spirochetosis (HIS) is defined as a colonisation of the apical membrane of the colonic mucosa and appendix by spirochetes, anaerobic filamentous bacteria[1].
It was first described by Harland & Lee in 1967. In humans, it has been associated with two species of spirochetes, Brachyspira pilosicoli (mainly asymptomatic, but sometimes as an opportunistic pathogen) and Brachyspira aalborgi (which may be pathogenic in humans more frequently than B. pilosicoli)[2],[3] They must be distinguished from the family Spirocochaetaceae (genus Treponema, Borrelia, Spirochaeta) and Leptospiraceateae (genus Leptospiraceae) which are not associated with HIS and which induce completely different pathological processes.
It is a very rare finding in our environment with a higher prevalence in less developed countries, above 40% in men who have sex with men and also in patients positive for human immunodeficiency virus (HIV)[4][4]. In Europe, there is an estimated prevalence of 2.5-9%[2]. Increased prevalence has also been reported in areas of poverty, in critically ill patients with multiple organ failure, and in coexistence with gonococcal infection[5]. Although the mechanism of transmission is not fully understood, it is suggested that faecal-oral transmission is most commonly implicated, followed by sexual transmission.
It is slow-growing and has specialised growth requirements, so it is not detectable in human faecal samples using routine diagnostic methods. However, it has been identified histologically attached to the colon and rectum in patients with conditions such as chronic diarrhoea, rectal bleeding and/or non-specific abdominal discomfort.
In this article we present the case of a patient with chronic diarrhoea secondary to intestinal spirochetosis, highlighting the importance of considering this aetiology among the differential diagnoses. understood, it is suggested that faecal-oral transmission is most commonly implicated, followed by sexual transmission.
It is slow-growing and has specialised growth requirements, so it is not detectable in human faecal samples using routine diagnostic methods. However, it has been identified histologically attached to the colon and rectum in patients with conditions such as chronic diarrhoea, rectal bleeding and/or non-specific abdominal discomfort.
In this article we present the case of a patient with chronic diarrhoea secondary to intestinal spirochetosis, highlighting the importance of considering this aetiology among the differential diagnoses.
Clinical Case
We present the case of a 57-year-old patient under study in the Digestive Department for diarrhoea of 5-6 liquid or soft stools without pathological products per day, of one year's duration. As personal history, the patient is being treated with enalapril and simvastatin for hypertension and dyslipidaemia. She has no family history of interest. She denies toxic habits. Native of Spain, she denies recent trips to developing countries. She had previously had sexual relations with only one stable partner, none in the last 5 years.
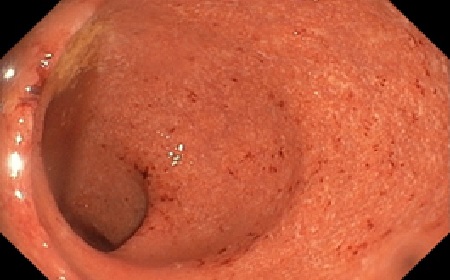
An analysis was performed with blood tests showing mild iron deficiency (IST 12%) without anaemia (Hb 12.4 g/dl) and stool analysis with stool culture, parasites and Cl. Difficile negative, with high levels of calprotectin (303 µg/g of stool).Subsequently, a colonoscopy was carried out which revealed multiple aphthous ulcers in the right colon up to the hepatic angle suggestive of non-specific aphthous colitis (infectious or inflammatory) and multiple biopsies were taken (Figure 1). Pathological anatomy showed active chronic colitis of infectious aetiology with the presence of filamentous microorganisms attached to the colonic mucosa compatible with intestinal spirochetosis (Figures 2 and 3).
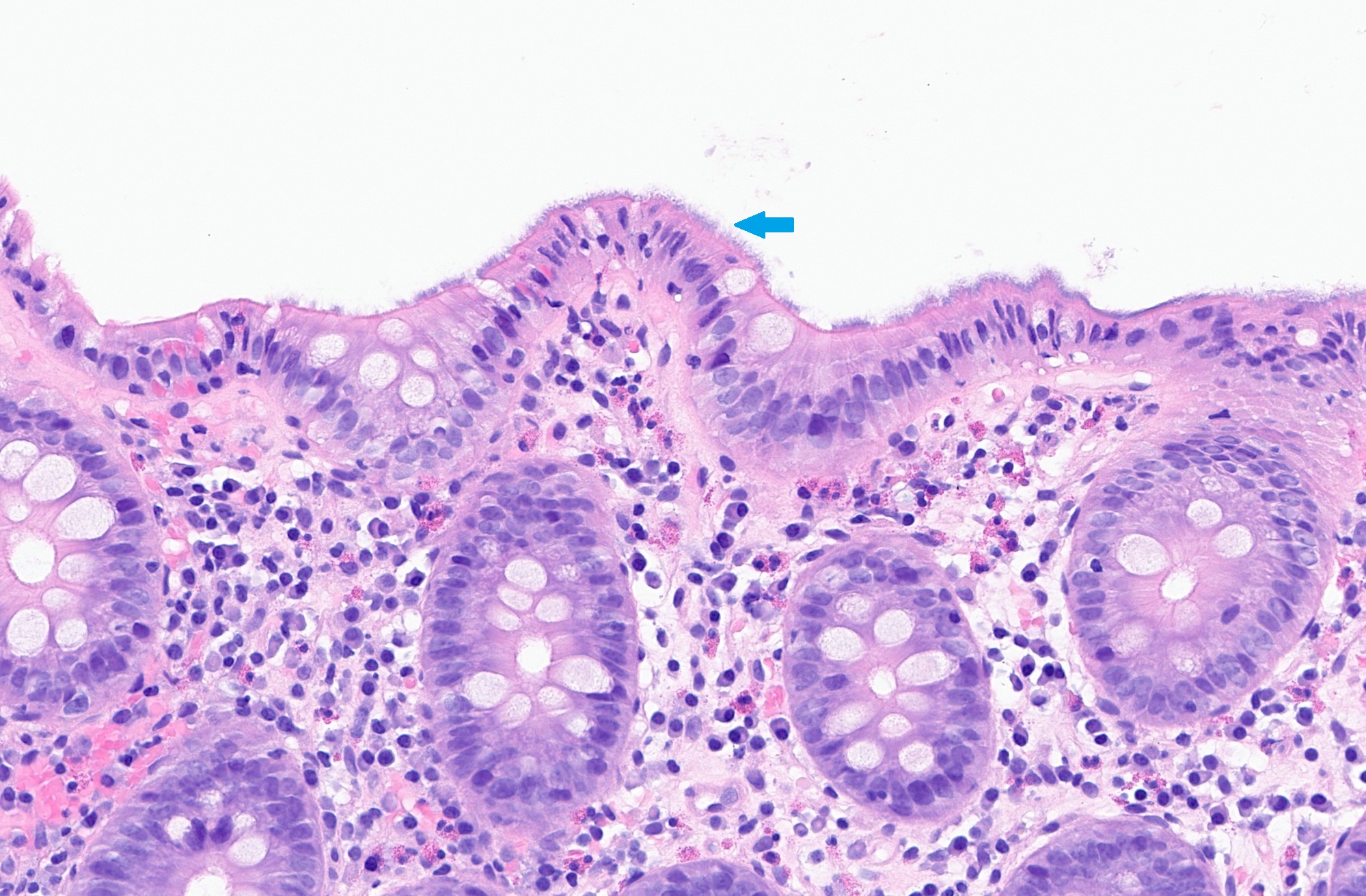
Figura 2
Tinción de Hematoxilina-Eosina 40x. Mucosa de colon en la que se aprecia una "falsa barrera epitelial” (flecha azul) en el borde en cepillo de la mucosa intestinal.
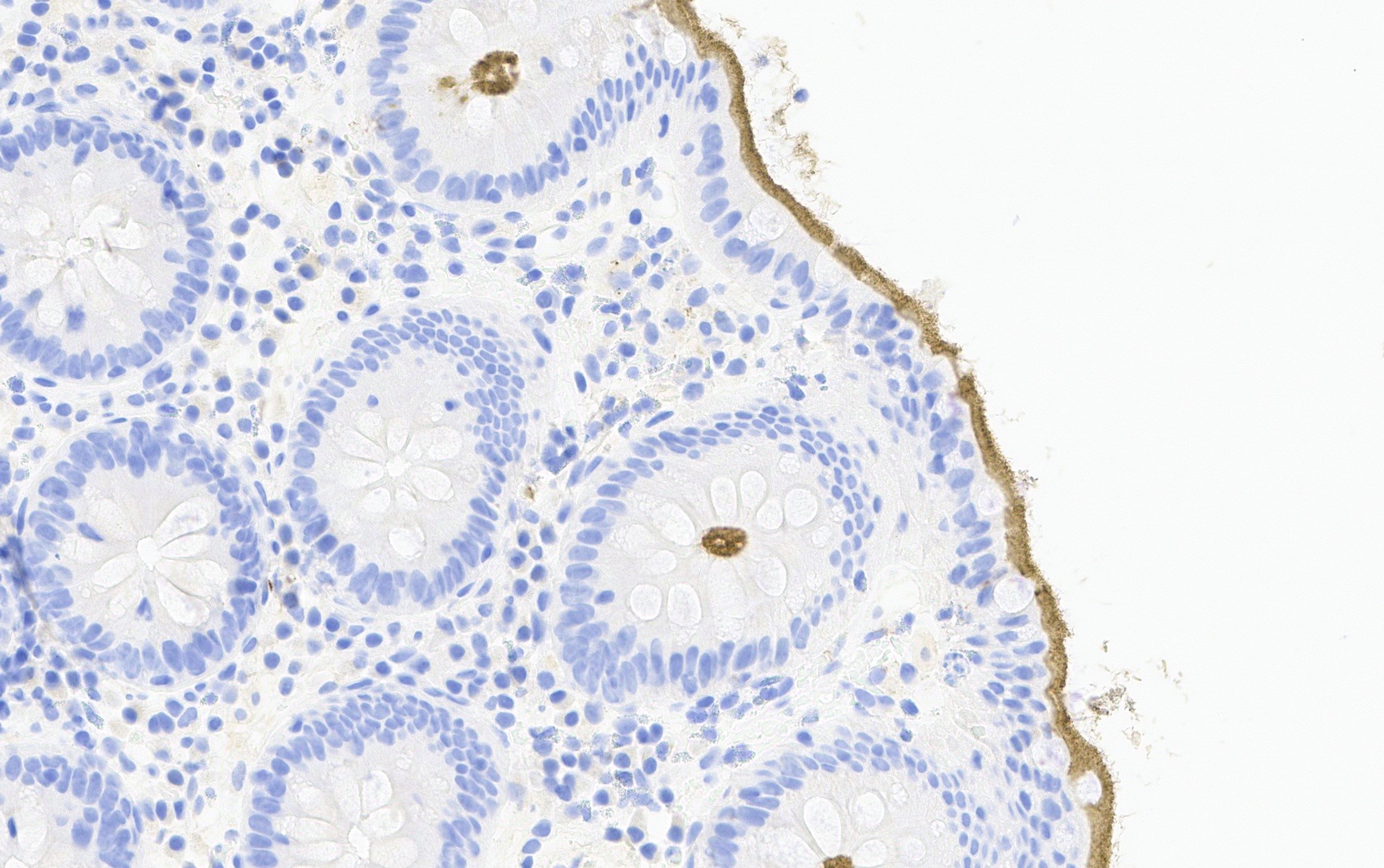
Figura 3
Inmunohistoquímica (40x). Técnica con anticuerpo anti-Treponema positiva para espiroquetas con microorganismos adheridos al borde de la superficie intestinal (en amarillo).
In view of these findings, complete serology was performed with treponemal and non-treponemal tests as well as tests for HIV and hepatitis B and C virus, with negative results.
Given that infection by treponema pallidum is the most common aetiology of intestinal spirochetosis despite negative serology for Treponema, in view of the pathological anatomy and the patient's clinical findings, it was proposed to start treatment with penicillin G benzathine for 3 weeks.
However, given the epidemiological context of the patient with an absence of risk factors for infection by treponema pallidum and no other data suggesting a syphilitic aetiology (absence of skin or eye lesions or involvement of the central nervous system), the atypical location of the aphthae in the right colon, which in the case of syphilis they are usually found in more distal segments of the intestine or in the rectum and the negative serology for Treponema, which has a high specificity and sensitivity, a slow incubation stool culture is requested to screen for other species of the spirochetes genus.
The patient was reviewed one month later and showed no clinical improvement with penicillin treatment. The results of the stool culture after the slow incubation were reviewed and found to be positive for Brachyspira. It was decided to start oral treatment with metronidazole (500 mg every 8h) for 10 days. After two weeks, the patient presented clinical remission of the symptoms, and control colonic biopsies subsequently confirmed the absence of filamentous microorganisms adhering to the colonic epithelium.
Discussion
HIS can affect the entire colon, the appendix and even the terminal ileum. Most cases of colonisation in humans by spirochetes spp. are asymptomatic. The most common form of presentation is chronic diarrhoea, although it may also manifest with abdominal pain, alternating bowel habits, rectorrhagia or spirochetemia (mainly in immunocompromised patients). It has also been reported in association with colonic intussusception.
Although the mechanism of transmission is not fully understood, it is suggested that oro-fecal transmission is most commonly implicated, followed by sexual transmission. Recent studies have shown that colonisation of the colonic epithelial surface or mucosal layers by pathogenic Brachyspira species was detected in 40% of IBS patients with diarrhoea[6],[7].
Diagnosis is made by identification of the microorganism on histological examination using specific techniques. The use of immunohistochemical (IHC) techniques with anti-T. pallidum antibodies is positive due to cross-reactivity with the genus Brachyspira. It is advisable to perform a stool culture with a slow incubation period to look for the growth of bacteria of the genus Brachyspira.
Other causes of diarrhoea; infectious and digestive absorption disorders, inflammatory bowel diseases and/or neoplastic diseases should be excluded before specific diagnostic techniques are requested. Differential diagnosis with Treponema Pallidum infection[8] should be made especially in men who have sex with men and in patients with HIV infection; by specific serology and evaluation of extraintestinal manifestations. The use of serological testing may be limited in patients with advanced immunosuppression and/or early disease.
Regarding treatment, a expectant attitude is recommended, reserving antibiotic treatment for those patients with persistent symptoms and no other demonstrable pathology. The treatments used are diverse, both in terms of dosage and duration, although metronidazole is the most commonly used. If treated, a follow-up biopsy is recommended to confirm eradication.
This case illustrates a controversial and extraordinarily rare cause of chronic diarrhoea, but should be considered in the differential diagnosis of this entity, especially in patients with predisposing risk factors.

 Descargar número completo
Descargar número completo Download full issue
Download full issue